I specialize in a technique of vasectomy that has been proven to reduce complications during- and after the operation:
No Scalpel
No Needle
Open-ended

No knife or surgical blade is used to cut the skin during the operation. I use only the “key-hole”- or “minimally invasive” surgical technique. This reduces pain and post-operative complications and facilitates faster recovery.

A needle is not used for local anaesthesia injection. I use a revolutionary “jet-spray”-instrument (MadaJet™) which delivers local anaesthetic fluid (lidocaine) into the skin without the need for a needle puncture. With this method, there is virtually no pain associated with the procedure.

The testicular end of the vas deferens is not tied but it is left open. This decreases the risk of developing “Post Vasectomy Pain Syndrome” and also improves the success rates of future vasectomy reversal, should a patient require it at a later stage.
Key Points: Vasectomy…
- Is a minor surgical procedure with few complications.
- Is intended to be a permanent form of contraception.
- Does not produce immediate sterility. It takes about 2 – 4 months before you can be sure that you are sterile by having a microscopic examination of your semen (semen analysis test). For this reason, another form of contraception must be used until the post-operative semen analysis confirms sterility.
- Does not cause erectile dysfunction (impotence), low levels of testosterone or a decrease in sex drive.
- Is not always 100% reliable in preventing pregnancy. Even after successful vasectomy has been confirmed on semen analysis, there is still about a 1 in 3000 risk of pregnancy.
- Options for fertility after vasectomy include microsurgical vasectomy reversal and in vitro fertilization.
- The rates of surgical complications such as symptomatic haematoma and infection are about 1%.
- Chronic scrotal pain / “Post Vasectomy Pain Syndrome” may occur in about 1% of patients after vasectomy.
- Having a vasectomy does not increase a man’s risk of developing prostate cancer, testis cancer, heart disease, stroke or dementia.
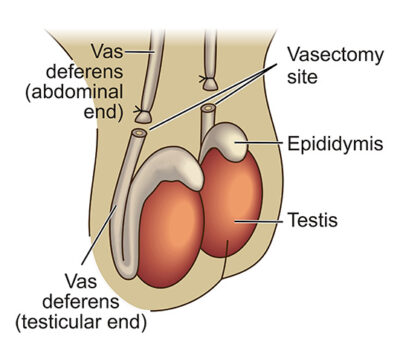
Basic Anatomy
Sperms are produced and stored in the testicles. During sexual intercourse at the time of male orgasm, the sperms are rapidly transported from the testicle and are ejaculated. The thin tube that transports the sperm from the testicle is called the “vas deferens”. Each testicle has only one vas deferens.
During the vasectomy procedure, the vas deferens from each testicle is cut through and one end (abdominal end) tied off. This prevents any future transport of sperms away from the testicle. In other words, sperms are still being produced but they have no way of getting from the testicle to “the outside”, therefore rendering the male infertile (sterile).
The Vasectomy Procedure Step-by-Step
The majority of men who opt to have a vasectomy do so between the ages of 25 and 50 years – this is usually a time of having lots to get on with at work and at home. With this in mind, I have optimized the circumstances and technique of the vasectomy procedure to ensure a relaxed and stress-free operation day and rapid post-operative recovery.
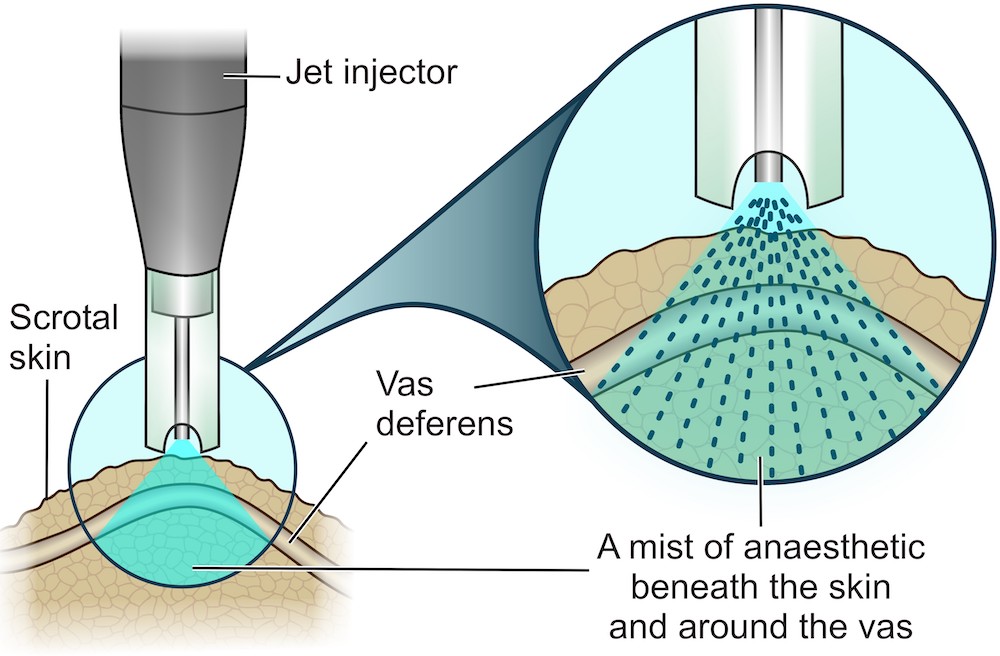
Step 1: Local Anaesthesia – NO NEEDLE
No needle is used to inject local anesthetic into the area that will be operated on. I use the “Madajet Needle-Free Injector” to spray a high pressure jet of long-acting local anaesthetic (lidocaine) solution onto the scrotal skin on the exact spot where access to the vas deferens will be obtained.
The mist of anaestetic penetrates into the skin and underlying structures (vas deferens), achieving a complete numbing effect 12 times faster than with the conventional needle-injection anaesthesia technique. Apart from the benefit that patients are not subjected to the pain of a needle puncture in this very sensitive area of the body, another advantage of the “no needle” approach is that there is less trauma to the small nerves and blood vessels lying under the skin and around the vas deferens. Minimizing tissue trauma during an operation facilitates a decrease in post-operative pain, fewer complications and faster recovery.
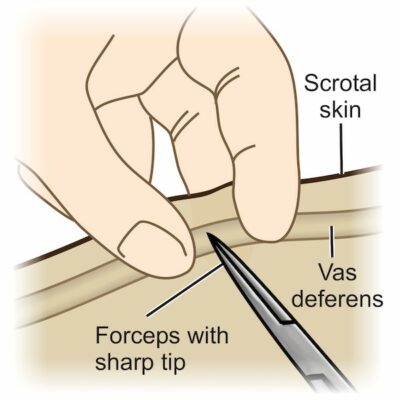
Step 2: Access to the Vas Deferens – NO SCALPEL
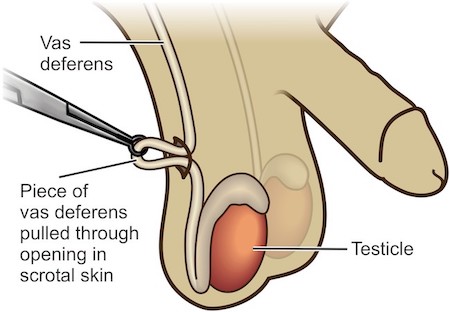
After making sure that the area has been completely anaesthetized, a small surgical forceps with a very sharp tip is used to puncture the skin overlying the vas deferens. The opening in the skin is then dilated / opened up a few millimeters to allow a segment of the vas deferens to be pulled through the opening – a special forceps with a ring at the tip is used for this purpose.
The majority of men who opt to have a vasectomy do so between the ages of 25 and 50 years – this is usually a time of having lots to get on with at work and at home. With this in mind, I have optimized the circumstances and technique of the vasectomy procedure to ensure a relaxed and stress-free operation day and rapid post-operative recovery.
Step 3: Removing a segment of vas and tying off one end only – OPEN ENDED
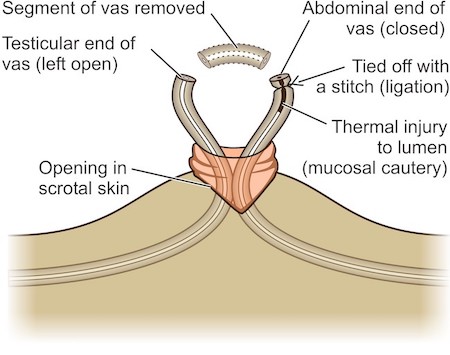
A 3cm piece of vas deferens is now pulled through the skin opening and a ± 1cm segment is cut out, using a surgical scissors. This leaves 2 open ends of vas deferens:
Abdominal end: The inside (lumen) of the abdominal end of the vas deferens is thermally disrupted (“mucosal cautery”) in order to prevent it from opening up and leading to vasectomy failure. The abdominal end is also closed by tying it with a surgical stitch (“ligation”). Furthermore, Performing these three measures (ligation, fascia interposition, mucosal cautery) ensures a very high success rate.
Testicular end: This end of the vas deferens is not closed with a stitch – it is left open (“Open-ended Vasectomy”). Leaving this piece open has been proven to reduce the risk of Post Vasectomy Pain Syndrome, which is a long-term painful and extremely bothersome reality for about 2% of men who are subjected to the traditional method of vasectomy.
International research has further showed that open ended vasectomy significantly improves the chances of successfully reversing the vasectomy, should patients change their mind and wish to have more children at some stage in the future.
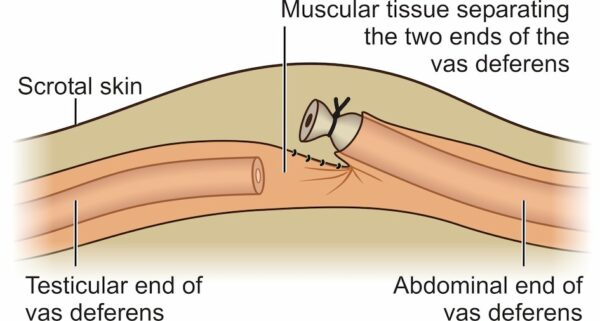
As an extra measure of safety to make sure that the vasectomy does not fail, I stitch a small piece of muscle tissue that is normally situated next to the vas deferens over the tied-off end – this technique ( “fascia interposition”) has been proven to decrease the risk of vasectomy failure even more.
It is important to note that open ended vasectomy (combined with ligation, fascia interposition and mucosal cautery of the abdominal end) is just as effective in establishing male sterility as a vasectomy where both ends of the vas are tied off. So no compromise is made on the efficacy of the vasectomy by leaving one end open – it just has the added advantages outlined above.
Steps 1 to 3 should take altogether about 15 minutes to complete on both sides (left and right testicles). No stitches are needed to close the “no scalpel” openings in the scrotal skin – a small plaster is simply placed over each wound.
After the procedure and once my nursing staff has ensured that you are feeling relaxed and not in pain, you’ll be allowed to go home.
Recovery: Do’s and Don’ts
- Better to take it easy for the first day or two. Go directly home after the operation and rest: elevate your feet. Plan to limit the time on your feet as much as possible for the first few days.
- The local anaesthetic will wear off within about 3 hours after the operation and I will provide you with a prescription for pain medication and anti-inflammatories.
- Locally applied ice packs in the first 24 hours as well as a tight scrotal support garment (like 2 pairs of tight-fitting underpants worn over one another) for a few days are very effective in preventing post-operative pain and swelling.
- You will usually be given sick leave for 3 days but you may return to work earlier if you feel up to it and provided that your occupation does not involve physical exertion (lifting of heavy objects, walking long distances, standing for long periods).
- You should avoid heavy physical activity for approximately 1-2 weeks and may resume sexual activity 1 week after the procedure.
It is very important that you continue to use another method of contraception for at least 2 months after the vasectomy AND until you’ve confirmed a sperm count of zero on a formal laboratory sperm count test.
Complications
Although vasectomy is a minor procedure, any surgery on the human body carries with it the risk of possible complications. A complication after vasectomy is uncommon. Even if it does occur, it is usually more bothersome than serious and is mostly managed conservatively (ie no surgical intervention required).
Vasectomy does NOT cause
It is usually reported that men who undergo vasectomy and their partners express greater enjoyment and spontaneity of sex. However, occasionally a man may experience sexual problems after vasectomy, but these almost always have an emotional / psychological basis. Counseling usually alleviates the problem.
The male hormone testosterone is produced in the testicle and is transported to other areas of the body via the blood. Testosterone is not transported in the vas deferens and therefore vasectomy will not cause any change in a man’s testosterone levels.
The Vasectomy Guideline Panel of the American Urological Association evaluated numerous research publications on the association between vasectomy and the abovementioned conditions. They concluded that vasectomy does NOT increase a man’s risk of developing any of these illnesses.
How successful is vasectomy?
Vasectomy an effective form of contraception in more than 99% of cases. When compared to other forms of birth control, it may well have the highest success rate, but it is still not 100% and pregnancy may occur after vasectomy.
The Vasectomy Guideline Panel of the American Urological Association has published a list of vasectomy techniques with a success rate of more than 99%: the No Needle, No Scalpel, Open Ended Vasectomy that I perform, is one of these recommended and approved surgical options.
The rare cases of vasectomy failure may be caused by the following:
Surgical failure
Failure of the surgeon to correctly remove a segment of the vas deferens is extremely uncommon. Some surgeons use a vasectomy technique where only a single opening is made in the scrotal skin and the vas deferens on both the left- and right sides are accessed through this single incision. It has been described that the surgeon may in some cases mistakenly remove 2 segments from one vas deferens, leaving the other side still intact and able to transport sperm.
The technique that I use involves 2 small openings in the scrotal skin – one over the left sided vas deferens and one over the right side. Making 2 separate openings prevents vasectomy failure due to the oversight described above.
Patient failure
Vasectomy does not make a man sterile immediately. Live sperms able to fertilize a female egg are often still present in the abdominal end of the vas deferens for several weeks after the vasectomy. For this reason it is absolutely essential for a couple to use an alternative form of contraception until sterility has been confirmed.
Between 2 and 3 months after vasectomy the first “Post Vasectomy Semen Analysis” (PVSA) should be performed. Only if this test shows no moving sperm, can the man be considered sterile and other forms of contraception be safely stopped.
Recanalization
This occurs when the severed ends of the vas deferens spontaneously grow back together, once again allowing the unobstructed transportation of sperm. This may occur weeks to years after vasectomy. Certain vasectomy techniques are known to have high recanalization rates and are not recommended by international experts.
I use the Open Ended vasectomy technique with Ligation, Fascia interposition and Mucosal cautery of the abdominal end. This technique is one of 3 which are all recommended by the American Urological Association, as they have the lowest recanalization rates (<<1%).