Vasectomy Reversal
Before discussing vasectomy reversal, let’s first say something about vasectomy itself.
Sperms are produced and stored in the testicles. During sexual intercourse at the time of male orgasm, the sperms are rapidly transported from the testicle and are ejaculated. The thin tube that transports the sperm from the testicle is called the “vas deferens”. Each testicle has only one vas deferens.
During the procedure of vasectomy, the vas deferens from each testicle is cut through and usually tied off. This prevents any future transport of sperms away from the testicle. In other words, sperms are still being produced but they have no way of getting from the testicle to “the outside”.
The “sperm transporting tube” or vas deferens is a thin and delicate structure: it has a diameter of about 3-4mm, but the inside “hollow area / canal” (also called the “lumen”) where sperms and fluid flow through, has a diameter that is often less than half a millimeter! When performing a vasectomy reversal, it is this extremely small lumen / canal that needs to be reconstructed. But more about these tiny structures later…
Vasectomy Reversal
Prior to the mid 1970’s vasectomy had been generally regarded as not reversible and attempts at reversal yielded very poor results. In 1973, before the introduction of microsurgical techniques, the results of 1630 vasectomy reversal cases performed by 542 urologic surgeons were analyzed: it showed that the surgery had been successful in only 20% of the cases and it was reported that pregnancy after reversal of vasectomy was a rare event. In 1975 some Urologists started using a microscope to perform vasectomy reversal surgery – over the following decades, the success rate of the operation improved dramatically to well over 90%.
When talking about vasectomy reversal, it is useful to have an idea of the structure of the organs involved, as well as a basic understanding of the terminology that we use.
As mentioned previously, sperm cells are produced in the testicles. A network of very small tubes connects the testicle with the epididymis and as the sperms are produced, they are transported through these small tubes and stored in the epididymis. The epididymis is made up of a single small tube that is rolled many times on itself. The epididymal tube gradually enlarges and eventually becomes the vas deferens.
Important Concepts
Why Microsurgery?
The American Society for Reproductive Medicine (ASRM) issued the following guideline: “Since it is seldom possible to determine pre-operatively if vaso-epididymostomy will be required in a man undergoing vasectomy reversal, only surgeons skilled in both vaso-epididymostomy and vaso-vasostomy should perform vasectomy reversal”
The anatomical structures involved in vasectomy reversal surgery are very small and delicate:
- The lumen / inside canal of the vas deferens which the Urologist has to re-connect during vasectomy reversal is often less than half a millimeter in size (0.4 – 1.5mm)
- The lumen / inside canal of the epididymis tube is less than 1/10 of a millimeter in size (0.08mm).
The sutures that should be used for vasectomy reversal are very thin:
- The recommended suture is a 10-0 nylon thread with a thickness of 0.02mm – barely visible to the naked eye.
- Although thicker sutures are easier for the Urologist to handle (especially if he is not using an operating microscope), they have the disadvantages of not providing a watertight seal and of causing scar tissue that may block the delicate tube a few weeks after the operation.
Microsurgery – 24X Magnification
Surgery is performed with magnification provided by a surgical microscope. This is a large piece of equipment which stands on a foot-piece on the floor of the operating theatre. The eyepieces (for Urologist and assistant) are positioned above the operating field. Some operating microscopes also project the magnified image onto a high definition flatscreen monitor, so that the scrub nurse and other theatre personnel can follow the progress of the operation.
Only a surgical microscope provides adequate magnification for vaso-epididymostomy.
Surgical Loupes – 4X Magnification
Loupes look like normal glasses which a surgeon puts on but they have special lenses which provide some magnification.
Loupe magnification does not provide adequate magnification for vaso-epididymostomy.
Prof Zarrabi uses an Operating Microscope for all his cases

Loupe magnification is not sufficient

It is certainly possible to re-connect the vas deferens using only loupe magnification or even no magnification, but these techniques have much lower success rates than microsurgical procedures.
It is, however, not possible to re-connect the vas deferens to the epididymal tube – simply because it is too small a structure to see and to work on without proper magnification (which is provided by the surgical miucroscope). The Urologist will only know during the operation if a vaso-epididymostomy is required (up to 60% of cases) and if he is not operating with a microscope he will not be able to perform the required procedure. The only option would then be to just continue with re-connection of the vas deferens – a useless exercise that is sure to fail in these cases because of the blockage in the epididymis tube which has not been dealt with.
To ensure the highest chance of success with your vasectomy reversal, an accurate and watertight reconstruction is essential. The exact location of every stitch must be controlled, whether the re-connection is to the vas deferens or the epididymis. Your Urologist must have the skill, knowledge and equipment to diagnose epididymal blockage (intra-operative semen analysis using an additional 400X magnification microscope) and to then modify the operation if required (vaso-epididymostomy in stead of vasovasostomy). If there is no epididymal blockage and only a simple vasovasostomy is needed, a precise two-layer closure using the appropriate suture materials should be performed.
Choosing a surgeon
As a patient, there are many things that you need to consider when choosing a surgeon. For one thing, the anatomical area of your body that is to be operated on is not just any area! You should feel confident that the person holding the surgical knife has been adequately trained. Also, your ability to have children and a future family is at stake – you need a doctor who is committed and qualified to give you the best chance possible. Money is also a factor: medical insurance usually does do not pay for this operation and you need to be sure that you are investing wisely. So be sure to ask your surgeon about some of the following aspects before deciding:
Vasectomy Reversal Surgery Step-by-Step
Reversing a vasectomy is not merely a matter of “reconnecting the tubes” – apart from the technical ability required from the surgeon performing the surgery, there are crucial decisions which need to be made during the operation. It is the ability of the surgeon to correctly combine all of these factors that will ensure the highest chance of success for you, the patient
The vasectomy reversal operation is started by making an incision into the skin of the scrotum just above each of the testicles. The incisions are usually about 20mm long but may be extended in complicated cases in order to free up more of the vas deferens. The area of the previous vasectomy is identified and the two tied-off ends of the vas deferens are exposed. The next step is to excise these closed-up ends – this will leave two healthy ends of vas deferens that can now be sewn back together.
But first the surgeon will have to make an important decision…
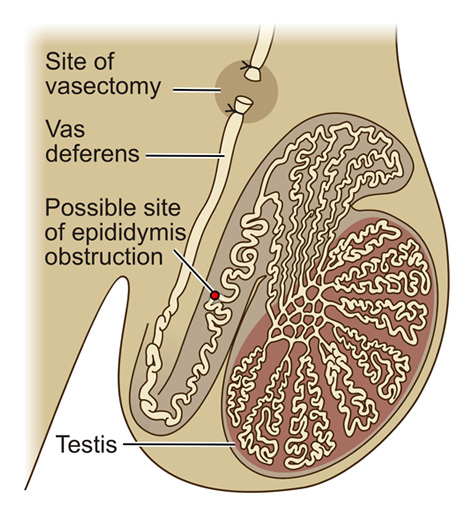
After a vasectomy, the testicles continue to produce sperms, but because the vas deferens had been tied off, these sperms cannot be transported away from the testicle and epididymis. The result is a build-up of pressure inside these structures. The epididymis is a very long and thin tube that is rolled on itself hundreds of times – over time, the pressure increase inside it will cause damage to the epididymis. This will eventually lead to blockage of the epididymal tube (Image 1). The longer the time since your vasectomy, the bigger the chance of you having damage and obstruction of the epididymis. And you’ve probably figured the rest out – there is no use re-connecting the vas deferens “downstream” if there is an obstruction in the epididymis “upstream” from it.
1. What are your chances of having epididymal obstruction?
This risk increases with time since your vasectomy, but even if your vasectomy was less than 5 years ago, you have about a 40% risk of epididymal obstruction. This risk increases to 75% if more than 10 years have passed since your vasectomy. Patients with epididymal obstruction need an operation that is completely different to the routine re-connection of the vas deferens!
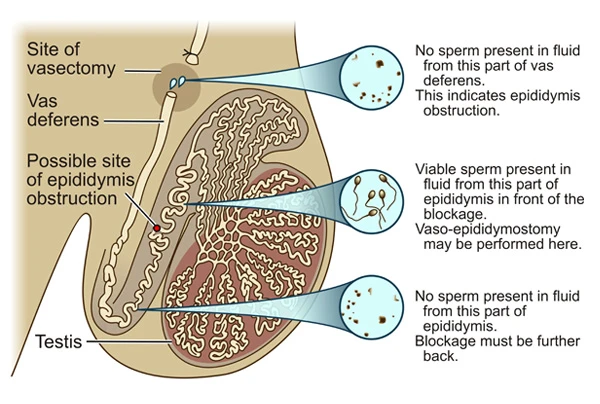
2. How will the surgeon know whether there is epididymal obstruction and what are the options if it is present?
Certainly, merely re-connecting the vas deferens will be a waste of time. The worrying thing is, that of all the surgeons who perform vasectomy reversal surgery, most do not have the instruments or skill to deal with epididymal obstruction. In these cases they will simply continue with re-connecting of the vas deferens and this is bound to fail. Epididymal obstruction is identified by microscopic examination of the fluid that comes out of the vas deferens on the testicle side. I do this examination myself in the operating room using a separate microscope with 400X magnification.
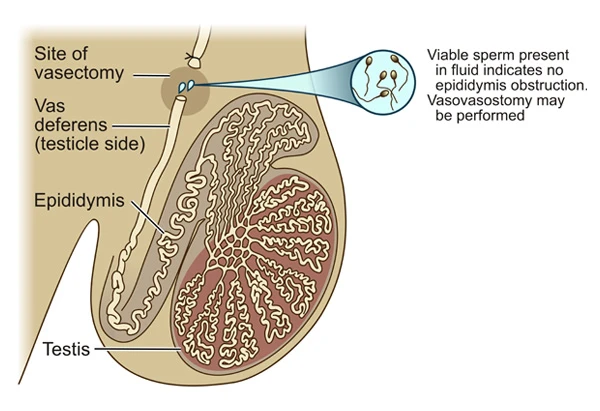
If sperms are present in this fluid (Image 2), I will continue with re-connecting of the vas deferens. If sperms are not present (Image 3), it means that there is an obstruction in the epididymis. In these cases, I will perform an operation to connect the vas deferens to the epididymal tube in an area in front of the blockage – this procedure is referred to as vaso- epididymostomy.
The American Society for Reproductive Medicine (ASRM) issued the following guideline:
“Since it is seldom possible to determine pre-operatively if vaso-epididymostomy will be required in a man undergoing vasectomy reversal, only surgeons skilled in both vaso-epididymostomy and vasovasostomy should perform vasectomy reversal”
3. Connecting vas deferens to vas deferens: Vasovasostomy
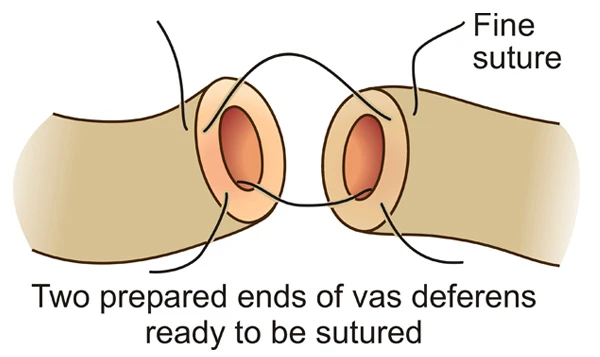
During the early stages of your vasectomy reversal operation, I will collect fluid from your vas deferens and examine it under a microscope with 400X magnification. The presence of sperms in this fluid will indicate that there is no obstruction in the epididymis, and in these cases I will continue to perform vasovasostomy. The two ends of the vas deferens that have been prepared are placed next to one another under the operating microscope that provides 24X magnification (Image 4).
Re-connection of the two ends is done in two layers to provide a watertight seal. The inside lumen / canal (diameter 0.4 – 1.5mm) is sewn first using a special 10-0 nylon suture (Image 5).
Although this suture is mostly used for very delicate eye- and heart surgery, leading micro-surgeons worldwide also use it for vasectomy reversal. The suture is barely visible to the naked eye and is only 0.02mm thick. Although this suture is very expensive, it has the major advantage of causing minimal inflammation, thus preventing the formation of scar tissue and subsequent blockage of the vas deferens after the vasectomy reversal operation. These complications are more common when thicker sutures are used.
4. Connecting vas deferens to epididymis: Vaso-epididymostomy
Epididymal obstruction is present in cases where microscopic examination of the vas deferens fluid shows no sperms (Image 3). If this is the case, I will proceed with the vaso-epididymostomy procedure.
The open end of the vas deferens is loosened up and brought into position next to the epididymis. The area of epididymal obstruction is identified and care is taken to connect the vas deferens to the epididymis in an area in front of the obstruction. The extremely thin epididymal tube (0.08mm) is identified and a small opening made into it. The vas deferens is then sewn to this opened tube, thus providing a passage for sperms and bypassing the site of blockage in the epdidymis (Image 6).
After completing the vasectomy reversal on the right and left sides, the scrotal skin incisions are closed. For this I use a suture that dissolves after about 3 weeks. A tight dressing is placed on the scrotum to prevent bleeding. You will be able to go home later that same day (ie no need to overnight in hospital) and will receive a prescription for pain medication. You will not be allowed to drive a car for the first 24 hours after the procedure, so be sure to have someone available to take you home from the hospital.
Because of the small size and delicate nature of the tissues involved, this operation is not quick to perform – in most cases it will take about 150 minutes (2,5 hours). Remember that reconstructions have to be done on the right and left sides, and each side involves a double layer closure with multiple stitches.
Because of the precision and concentration required, I do a maximum of only two of these cases per day. A micro-surgeon should never be rushed!
Because of the long duration of this procedure I absolutely prefer my patients to be under general anaesthetic. Some surgeons may offer vasectomy reversals under local anaesthetic or conscious sedation only – these are mostly colleagues who do not use the operating microscope.
The anaesthetists fee for sedation only (“twilight anaesthesia”) is not significantly less than for a general anaesthetic. During a microsurgical vasectomy reversal my patient needs to lie absolutely still for the entire duration of the surgery. Because it is a long procedure (2,5 hours), an awake patient is bound to become uncomfortable and restless. Even the slightest movement at a crucial moment may compromise the success of the operation.
I use only specialist anaesthetists who have many years of experience. These specialists have undergone years of intensive training in an academic hospital and obtained a specialist degree from a reputable university. They are highly trained to deal with any kind of situation that may arise while you are asleep in the operating theatre. I do not compromise on quality in this regard, because as a patient your life is literally in their hands!
You should take it easy for the first few days after the operation and will usually be booked off from work for one week. Locally applied ice packs in the first 24 hours as well as a tight scrotal support garment for a few days, are very effective in preventing post-operative pain and swelling. I will provide you with a prescription for pain tablets as well.
You should avoid heavy physical activity for approximately 3-4 weeks – remember that this operation is performed on very delicate structures which need time to heal and to regain adequate strength in the areas where the reconstructions had been performed. For this reason, you should also abstain from sexual activity for at least 3 weeks following the operation.
Sperm analysis tests are done at 3 months, 6 months and 12 months after the operation. The tests will provide us with valuable information regarding the success of the operation and the quality of the sperm.
Vasectomy reversal is generally a safe procedure. Complications are very uncommon and in the unlikely event that they do arise, conservative (non-surgical) management is successful in almost all cases.
Bleeding:
There is very little bleeding during the operation. It is also quite uncommon to have bleeding on the inside of the scrotum (wound hematoma) in the days following your surgery. However, should this occur, management will usually involve a course of antibiotics and anti-inflammatory medication, as well as tight-fitting scrotal support. Most hematomas will resolve on their own and there will be no long-term effects. It is important that you take it easy for the first few days after your surgery in order to further reduce the risk of a wound hematoma.
Infection:
Once you are asleep in the operating theatre, the anaesthetist will inject you with an antibiotic – this is standard for all surgical procedures and is sufficient to prevent infections after vasectomy reversal. There is no benefit in routinely taking an additional full course of oral antibiotics after your operation – in fact, this practice increases the resistance of germs to antibiotics. Wound infections may rarely occur after vasectomy reversal, and will usually be managed with a course of oral antibiotics.
Failure of the operation:
There is no Urologic surgeon in the world that will give a 100% guarantee of success for vasectomy reversal. Even if the operation itself was successful (resulting in a patent vas deferens and sperms present on post-operative semen analysis), it is still not a guarantee that your female partner will become pregnant (“Patency rate” vs “Pregnancy Rate” – see Terminology). You and your partner have to take the risk of failure of the operation – even though it is relatively small – into consideration before making a decision about vasectomy reversal. It is very important to me that my patients have realistic expectations of the outcomes of this procedure. (See “Success Rates”).