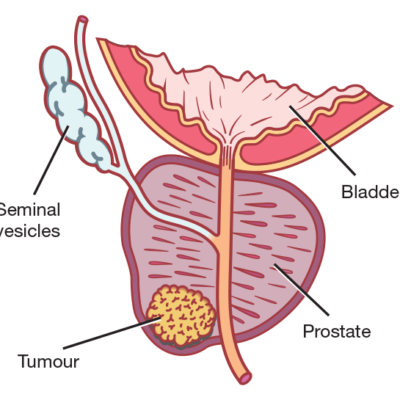
Worldwide, prostate cancer is the most common cancer that affects men. New Zealand is no different.
In my practice, I manage all aspects related to prostate cancer and the treatment thereof. This includes:
- Prostate biopsies – either trans-rectal ultrasound-guided (TRUS) biopsies or transperineal MRI-based fusion biopsies.
- Discussion of all available treatment modalities.
- Surgical treatment: Radical prostatectomy.
- Hormonal treatment.
- Active surveillance.
- Watchful waiting.
- Referral to other specialists as needed: Radiation Oncology, Medical Oncology etc
In some cases, prostate cancer is not a very aggressive cancer and men may live for years after being diagnosed. However, in other cases, it may be a more aggressive disease and require major surgery or other treatments.
How is prostate cancer diagnosed?
1. Symptoms
Most men with prostate cancer have no symptoms as prostate cancer causes symptoms only when it is advanced. In such cases, it may cause low back pain or difficulty with urination. All men who have difficulty with urination do not necessarily have prostate cancer. A non-cancerous enlargement of the prostate, also known as benign prostatic hyperplasia (BPH), is much more common and often causes difficulty with urination.
2. Blood test (PSA)
Prostate Specific Antigen (PSA) is a blood test that is used to identify patients at risk of having prostate cancer. Patients with high PSA have a higher risk of prostate cancer. A doctor needs to help you to interpret the PSA test as the PSA count can sometimes be high in non-cancerous conditions.
3. Finger test called Digital Rectal Exam (DRE)
An index finger is placed into the anus to feel the prostate. This enables assessment of prostate size, consistency (hard or soft) and the presence of nodules (lumps).
4. Prostate biopsy
Prostate biopsy is done by inserting an ultrasound guided biopsy probe (more or less the size of an index finger) into the anus and then taking small pieces of the prostate for pathology examination in a laboratory. Previously all prostate biopsies were done via the trans-rectal route, nowadays we are moving more towards trans-perineal prostate biopsies using MRI images of the prostate to target specific lesions. This is the most accurate test for making a diagnosis of prostate cancer. Prostate biopsy is usually done under local anesthesia; it can also be done under general anesthesia depending on your personal preference and also your medical insurance.
After the prostate biopsy, the samples of prostate tissue taken during biopsy are sent to a pathologist who determines the presence or absence of prostate cancer as well as the aggressiveness of cancer. The detailed pathology report is essential to appropriately advise you about the treatment options.
What are the risks of a prostate biopsy?
1. Infection
Infection of the prostate or urinary tract can occur after biopsy but it is uncommon and only occurs in about 1 to 5 out of every 100 men who undergo prostate biopsy. The signs of infection include fever, nausea, chills, severe pain in the area of the anus and painful urination. You will receive an antibiotic before and after biopsy to reduce the chance of getting infection. If you develop these symptoms after biopsy, contact your GP or Emergency Department urgently for appropriate advice.
2. Bleeding
Passage of blood in the stool and urine is not unusual after prostate biopsy and usually stops without any treatment. Heavy bleeding after prostate biopsy is extremely rare.
3. Blood in the semen
Some patients report blood staining of semen after prostate biopsy. In some occasions this may persist for 4-6 weeks and will also resolve spontaneously.
What are the options for treatment of prostate cancer?
The appropriate treatment of prostate cancer depends on many factors:
- The size and aggressiveness of your cancer.
- The degree of advancement / spread of the disease.
- Your general health.
All of this will be discussed with you to help you and your family make the best choice based on your individual circumstances.
In general, the treatment options for prostate cancer include:
1. Surgery: Radical prostatectomy
Surgical removal of the prostate with the aim of total cure of prostate cancer. Prostate cancer surgery is done for patients with cancer that has not spread to the rest of the body and who are healthy enough to withstand a big operation.
2. Radiation therapy: External beam
Radiation of the prostate with the aim of total cure of prostate cancer. The advantage above surgery is that you do not need to undergo a big operation. However, radiation therapy is not without potentially serious risks and side-effects.
3. Radiation therapy: Brachytherapy
This is a form of radiotherapy where small beads of radioactive materials are inserted into the prostate to kill cancer cells. Not all men are good candidates for this type of treatment.
4. Active surveillance (AS)
In order to qualify for this treatment option, you need to have a non-aggressive type of prostate cancer, which will be identified on prostate biopsy. Active surveillance involves regular follow-up with blood tests (PSA), MRI-scans and repeat prostate biopsy. Some men on AS will require definite treatment of their prostate cancer somewhere down the line whilst others may never require treatment.
5. Watchful waiting (WW)
This treatment modality is mostly reserved for men with advanced prostate cancer or men of advanced age. In general, treatments are only given if symptoms develop, cancer spread is detected (metastases) or if PSA levels go very high.
6. Hormonal treatment
Prostate cancer cells depend on male hormones such as testosterone for growth. Removal of testosterone from the body slows down the growth of prostate cancer. In men with high-risk prostate cancer or advanced prostate cancer, medications and injections can be given to stop testosterone production in the body. This will usually slow down the prostate cancer and decrease the PSA level.
7. Chemotherapy
Chemotherapy is mostly used for patients with advanced prostate cancer where other treatment options have failed.